Introduction to Pharmacogenomics
Several factors may contribute to how an individual can respond to medications such as gender, age, and diet. However, a person’s unique genetic makeup can also provide insight into how they may respond to medications. Pharmacogenomics is the compilation of research involving the relationship between genetic variations and how individuals can potentially respond to medications.1 In an article published by the Mayo Clinic stated “Precision medicine aims to customize healthcare, with decisions, and treatments, tailored to each individual in every possible way. Pharmacogenomics is part of precision medicine.2” That is a compelling argument that having a person’s Pharmacogenetic (PGx) profile would be beneficial to leverage when making decisions about medication selection. Pharmacogenetic (PGx) testing provides medical practitioners with a key diagnostic tool that can help them make more educated decisions about medications for their patients. The implementation of a PGx test as a standard of care in clinical practice can potentially save time, money, and unwanted side effects for patients.
Basic Overview of Genes
To comprehend genetics, there needs to be a basic understanding of DNA. It is easiest to think of DNA as a code that utilizes the letters A, C, G, and T to comprise its many genes. Different combinations of these letters signify the instructions those genes utilized to produce proteins in the body. Proteins are made up of amino acids sequenced from a corresponding gene. Proteins carry out many different functions of the body and one of those functions is the breakdown of medications (CYP450 enzymes). The presence of genetic variations in the genes can impact the instructions needed to produce these enzymes, affecting how individuals respond to medications.3Another way to label physical characteristics determined by genetic variants (medication metabolism) is the phenotype.4 There are typically five ways to identify pharmacogenomic phenotypes in PGx testing they are as follows: Poor Metabolizer, Intermediate Metabolizer, Normal Metabolizer, Rapid Metabolizer, and Ultra-Rapid Metabolizer. These phenotypic labels can foreshadow how medications can be broken down in the body or activated. Low enzymatic activity may prevent a patient from metabolizing medications like antidepressants and antipsychotics. When the drugs remain in the system too long, they can cause serious side effects. In contrast, in those with high levels of enzymatic activity, medications can break down too quickly resulting in no therapeutic benefit.
An example can be illustrated in the CYP2D6 enzyme where its phenotypic label is identified as a poor CYP2D6 metabolizer. If a patient were prescribed Paroxetine (Paxil) as initial therapy for their depression and they had a poor metabolizing function at the CYP2D6 enzyme they could potentially have a higher plasma concentration of Paroxetine in the blood increasing the probability of side effects. Having this information prior to prescribing can help prevent the occurrence of side effects or adverse events.
Pharmacogenetic (PGx) Testing Helps Clinicians Practice Precision Medicine
How can pharmacogenetics tests be helpful to doctors?
Pharmacogenetic (PGx) testing helps doctors pinpoint how well the body uses medications, allowing them to personalize choices on drugs. Precision medicine is the direction that healthcare practitioners are taking when evaluating their patient's cases. Pharmacogenetic (PGx) testing can play a pivotal role in the diagnostic element of precision medicine treatment plans.
There are currently more than 350 therapeutic agents recognized by the Food and Drug Administration that have package insert information that pertains to pharmacogenomic biomarkers. These pharmacogenomic biomarkers present actionable genetic information that can be used by healthcare practitioners to help personalize the selection of a drug for their patients.5 If this information is not used when making decisions about medication selection for patients’ liability implications can arise for clinicians. A study published in 2015 entitled “Pharmacogenomics in the clinic” estimated that of the 1200 commonly used FDA medications, which accounted for roughly four billion prescriptions, 18% (720M) were affected by actionable pharmacogenetic variables.6
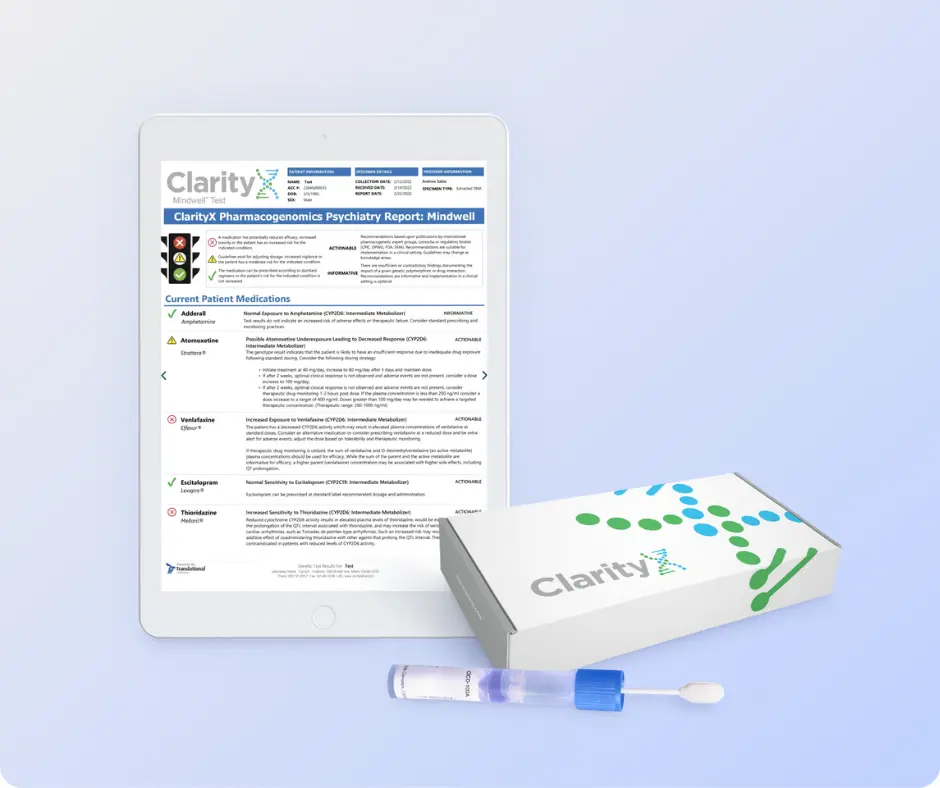
Healthcare practitioners and patients may be curious about the process of their first pharmacogenetic (PGx) test. ClarityX provides a seamless in-home testing experience. Simply visit our testing options page, select the test option from the menu and complete the checkout process. Once the kit is received follow the package instructions, perform a simple cheek swab, then mail the sample back using the prepaid envelope. The sample is then sent to the lab for processing and providers receive the results in 7-14 days on average. One of the most important facts about pharmacogenetic (PGx) testing is the results can be reevaluated for future medication changes as this test does not have to be repeated for those specific genes tested. In other words, pharmacogenetic (PGx) testing can provide a lifetime of knowledgeable decisions about medication selection for health care teams.
Relevant Pharmacogenomic Medical Conditions
(oncology, pain management, psychiatry, and cardiology)
One of the questions that puzzle your healthcare provider, especially those who treat cancer, is why some drugs work better for some patients but have no effect in others with the same cancers. Many cancer medications must be “switched on” to work. This turning on of a drug is known as activation, which is facilitated by enzymes. If the enzymes do not respond, the therapy will not be effective in fighting cancer. Pharmacogenomics testing can provide oncologists opportunities to personalize cancer treatments for their patients and has been used for many years to do so. Oncologist battle with the burden of addressing the many side effects that oncology medications can produce such as nausea, pain, depression, neuropathy, and infections. It is crucial for these patients to obtain optimization of their medication therapies so that responses to their oncology medication yield the most benefit. Supporting evidence is abundant for the utilization of pharmacogenomic (PGx) testing by oncologists. Some of the most actionable areas of study for oncology patients can be used when evaluating neuromodulators, antidepressants, pain, and antifungal medications. Pharmacogenomic results can be utilized all the way through the many stages of oncology treatment including palliative care. In the final stages of someone’s journey in their battle with cancer, providers want to be able to ensure that medications are effective in providing relief to their patients. Pharmacogenomic information specific to an individual can aid an oncology health care team in making the most informed decisions about medications for their patients.7 Pharmacogenomic (PGx) testing may help improve therapeutic benefits in pain management. The inability to achieve pain control with certain medications can leave some patients struggling, misusing, and discontinuing medications because of undesirable side effects. Through pharmacogenetics (PGX) testing, the healthcare practitioner might find that adjusting dosages or changing therapies may be warranted to optimize medication therapy and avoid undesirable side effects. In addition, if a patient is taking pain medicine and getting little relief, there can be a tendency on the patient’s part to increase the dosage leading to the potential abuse of the medication. This can lead to toxic levels of the drug in the body increasing the likelihood of addiction, and possible overdose. Pharmacogenomic (PGx) testing can help mitigate the threats of these complications and simplify the choices of medications for patients. An example of where pharmacogenomic (PGx) testing can provide insight into the metabolism of pain medications is with the CYP2D6 enzyme. Medications such as hydrocodone, oxycodone, tramadol, and codeine are all affected by the metabolizing actions of CYP2D6. Having pharmacogenomic information on this enzyme in pain management can provide insight if a patient should even begin these therapies or change these therapies reducing the risk of unwanted side effects or abuse of opioids. Pharmacogenomics is not limited to opioid treatments, there is also supporting pharmacogenomic evidence with NSAIDS where CYP2C9 or CYP2C8 are major contributors to their metabolism. Polymorphisms from these CYP450 enzymes can all contribute to difficulties in drug selection for pain management patients and are utilized as a standard of care in this space.8
Psychiatry is one of the most profoundly affected areas of study in pharmacogenomics. When beginning therapy for any mental health condition it is well documented that most therapies can take four to six weeks to provide relief from mental health symptoms. Many times, healthcare practitioners are forced to use the trial-and-error method for selecting medications. This can slow the progress of relieving the symptoms patients may be experiencing or potentially increase symptoms in the process of beginning new therapies. This is where pharmacogenomic (PGx) testing can provide a more focused direction for patients being treated with mental health conditions. To better predict how a patient will react to medications in mental health it is important for a patient’s healthcare provider to have knowledge of how the metabolism of medications can be affected by their genetics. For example, selective serotonin reuptake inhibitors (SSRI) are a commonly prescribed class of antidepressants for individuals battling with depression and anxiety disorders. The enzymes CYP2D6 and CYP2C19 can both contribute to the metabolism of SSRI’s which can lead to a patient potentially experiencing unwanted side effects or no benefit at all. Since medications like SSRI’s can take up to four to six weeks to achieve any therapeutic benefit, it is of the utmost importance to initiate the most effective therapy to start. Pharmacogenomic (PGx) test results are crucial in selecting the right medication for mental health patients and can be revisited repeatedly to make the most informed decision about their medications. 9
Cardiology treatments are yet another area that pharmacogenomic (PGx) testing can provide insight into drug selection for patients. There are many therapies used for the treatments of hypertension, stroke, and heart attack that can be affected by a patient’s metabolism of certain medications. For example, clopidogrel (Plavix) is a common platelet P2Y12 receptor inhibitor prescribed to decrease plaque buildup in the arteries ultimately preventing patients from having a cardiac event like a heart attack. Clopidogrel is unique in its metabolism by CYP2C19 in that it requires activation by this enzyme. Therefore, if a patient has a poor metabolizing function of CYP2C19, clopidogrel is not able to be activated in the body and cannot provide any protection against a heart attack. The FDA drug label for clopidogrel warns that patients that are identified as poor CYP2D19 metabolizers should begin other anti-antiplatelet therapies not metabolized by CYP2D19. 10
Pharmacogenomic (PGx) Testing Impact on Patients and the Healthcare System
Evidence and research support the implementation of pharmacogenomics as a standard of care in precision medicine. In a meta-analysis conducted by Victoria David in 2021, it states, “It is estimated that 95% of the population are estimated to carry at least one genetic variant that is discordant with at least one medication.” In addition, the meta-analysis showed that all-cause hospitalization occurred significantly less frequently in the PGx tested arm than in the treatment-as-usual arm of the study.11 Pharmacogenomic (PGx) testing is a highly informative diagnostic tool that can reduce the likelihood of adverse drug reactions, adverse drug events, and potential hospitalization of patients. Selecting the right medications initially can have a profound impact financially on the health care system. A study conducted in 2016 evaluating how prescription drugs can affect healthcare annual costs deduced that an estimated 275,000 lives are lost, and $528.4 billion dollars are wasted due to avoidable illness and death resulting from non-optimized medication therapy.12
Hope for the Future
Precision medicine is the way of the future for health care where pharmacogenomics seamlessly can be implemented. The more healthcare practitioners become educated about the benefits of Pharmacogenomics (PGx) testing, the inevitable implementation into their own practice is achievable. Patients have the right to have the most informed decisions made about their medications. This can prevent so many complications that taking medications can usually produce. Imagine a world where a patient visits a healthcare provider with a medication complaint, and pharmacogenetics (PGx) testing is routine. In this scenario, the doctor would order a pharmacogenetic test with other lab tests, and the resulting report could provide a road map for treatment based on the patient’s genetics. Pharmacogenetics testing is beginning to become a standard of care by many medical practices and will continue until its universally used.
1 PHARMGKB, 202. https://www.pharmgkb.org/
3 https://www.pharmgkb.org/whatIsPharmacogenomics
4 https://www.pharmgkb.org/page/glossary#pharmacogenomics
6 Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature. 2015 Oct 15;526(7573):343-50. doi: 10.1038/nature15817. PMID: 26469045; PMCID: PMC4711261.
7 Patel, Jai N., et al. “Value of Supportive Care Pharmacogenomics in Oncology Practice.” The Oncologist, vol. 23, no. 8, 2018, pp. 956–964., https://doi.org/10.1634/theoncologist.2017-0599.
8 Peiró, Ana M. “Pharmacogenetics in Pain Treatment.” Pharmacogenetics, 2018, pp. 247–273., https://doi.org/10.1016/bs.apha.2018.04.004.
9 Hicks, JK, et al. “Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline forcyp2d6andcyp2c19Genotypes and Dosing of Selective Serotonin Reuptake Inhibitors.” Clinical Pharmacology & Therapeutics, vol. 98, no. 2, 2015, pp. 127–134., https://doi.org/10.1002/cpt.147.
10 https://www.pharmgkb.org/labelAnnotation/PA166104777
11 David, Victoria, et al. “An Analysis of Pharmacogenomic-Guided Pathways and Their Effect on Medication Changes and Hospital Admissions: A Systematic Review and Meta-Analysis.” Frontiers in Genetics, vol. 12, 2021, https://doi.org/10.3389/fgene.2021.698148.
12 Watanabe, Jonathan H., et al. “Cost of Prescription Drug–Related Morbidity and Mortality.” Annals of Pharmacotherapy, vol. 52, no. 9, 2018, pp. 829–837., https://doi.org/10.1177/1060028018765159.